By Kiran Thakur, MD

Kiran Thakur
Before the introduction of the measles vaccine in the United States in 1963, more than 500,000 cases of measles and at least 500 measles-associated deaths were reported annually1,2. Although measles elimination was declared in 2000, importations of cases from endemic areas of the world continue to occur, leading to secondary measles cases and outbreaks. This year, the United States is experiencing a record number of confirmed measles cases, with 592 cases and 18 outbreaks reported to the Centers for Disease Control’s (CDC’s) National Center for Immunization and Respiratory Diseases (NCIRD) between Jan. 1 and Aug. 29, 20143. (See Figure 1.) Recent increases in the incidence of measles in the United States are attributed to the importation of measles virus through travel to other countries, including the Philippines, where there is a large, ongoing measles outbreak. Approximately 20 million cases of measles occur each year globally, and importations into the United States continue to pose a risk for measles cases and outbreaks. This is also coupled with greater rates of transmission because of unvaccinated or incompletely vaccinated United States citizens, a significant portion of which are children4.
The large number of cases this year emphasizes the need for health care providers to have a heightened awareness of the potential for measles and the importance of vaccination to prevent infection, in particular in young children and travelers who are susceptible to severe infection. Health care providers should maintain a high level of suspicion for measles among febrile patients who present with rash, cough, coryza, and/or conjunctivitis. Patients should be asked about recent travel abroad and/or contact with returning travelers, and their vaccination status.
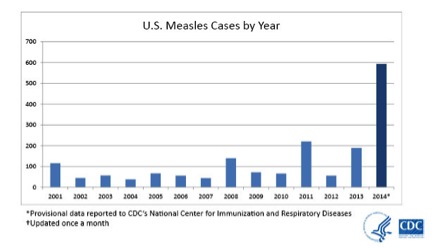
Figure 1. United States (U.S.) measles cases by year.
In particular, neurologists should be aware of the early and late neurological manifestations of the infection. Although neurological symptoms and signs have not been reported among the 592 cases in the United States reported this year, neurologists should be aware of the potential early and late central nervous system (CNS) complications of the infection. CNS manifestations are indeed rare, but devastating when they occur. The most common CNS manifestation of measles infection is acute measles encephalitis (AME) occurring in approximately 0.1 percent of cases5. In AME, the virus replicates within neurons and triggers a lymphocytic infiltration within the brain parenchyma and meninges6. AME typically occurs during the exanthem phase of the systemic illness, but can rarely precede the onset of rash. Cerebrospinal fluid (CSF) typically shows a lymphocytic pleocytosis and mildly elevated protein7. Treatment for AME is largely supportive and prognosis is guarded as approximately 20 percent of patients die, with at least one quarter of survivors developing permanent neurologic sequelae8. Post-measles encephalomyelitis (PME) occurs in approximately one in 1,000 patients, occurring within two weeks of the onset of rash and is characterized by seizures and focal neurological deficits. Periventricular demyelination, induction of immune responses to myelin basic protein, and absence of measles virus in the brain suggest that PME is an autoimmune disorder triggered by measles virus infection9. Other CNS complications that occur months to years after acute infection are measles inclusion body encephalitis (MIBE) and subacute sclerosing panencephalitis (SSPE), both of which are caused by persistent measles virus infection. MIBE is a rare, but fatal complication associated with progressive neurological deterioration that affects individuals with defective cellular immunity and typically occurs months after infection. SSPE is a rare delayed complication of measles that occurs in about one in 10,000–100,000 patients and is characterized by seizures and progressive deterioration of cognitive and motor function followed by death 5–15 years after measles virus infection10. On histopathology, neurons, oligodendrocytes, astrocytes and microvascular endothelial cells are infected11. SSPE most often occurs in people infected with measles virus before two years of age.
Rates of CNS manifestations due to measles infection have dramatically declined since the introduction of the measles vaccine, though with the resurgence of measles outbreaks around the world, and the increase in refusal of vaccines in resource-rich nations, the risk of these complications is now heightened. As travel to worldwide destinations becomes more accessible, neurologists should be aware of the potential neurological effects of acquired infections abroad, including measles and other neurotropic infections. Clinicians should also be aware of the increasing susceptibility to infection in those who are not vaccinated, including young children.
References:
1. Campbell H, Andrews N, Brown KE, et al: Review of the effect of measles vaccination on the epidemiology of SSPE. Int J Epidemiol 36: 1334-1348, 2007 4
2. Hinman AR, Orenstein WA, Papania MJ: Evolution of measles elimination strategies in the United States. J Infect Dis 189(suppl 1):S17-S21, 2004
3. http://www.cdc.gov/measles/hcp/index.htm Accessed September 4th, 2014
4. Verla-Tebit E, Zhu X, Holsinger E, et al. Predictive value of immunization records and risk factors for immunization failure in internationally adopted children. Arch Pediatr Adolesc Med 2009;163:473-479
5. Schneider-Schaulies J, Meulen V, Schneider-Schaulies S. Measles infection of the central nervous system. Journal of Neurovirology 2003;9: 247–252
6. Johnson RT, Griffin DE, Hirsch RL, et al: Measles encephalomyelitis—clinical and immunologic studies. N Engl J Med 310:137-141, 1984
7. Johnson RT, Griffin DE, Hirsch RL, et al: Measles encephalomyelitis—clinical and immunologic studies. N Engl J Med 310:137-141, 1984
8. Perry RT, Halsey NA: The clinical significance of measles: A review. J Infect Dis 2004;189(suppl 1):s4-s16
9. Johnson RT, Griffin DE, Hirsch RL, et al. Measles encephalomyelitis—clinical and immunologic studies. N Engl J Med 1984; 310: 137–41.
10. Bellini WJ, Rota JS, Lowe LE, et al. Subacute sclerosing panencephalitis: more cases of this fatal disease are prevented by measles immunization than was previously recognized. J Infect Dis 2005; 192: 1686–93.
11. Allen IV, McQuaid S, McMahon J, et al. The significance of measles virus antigen and genome distribution in the CNS in SSPE for mechanisms of viral spread and demyelination. J Neuropathol Exp Neurol 1996;55:471–480.
Thakur is a post doctoral fellow with the Division of Neuroinfectious Diseases and Neuroimmunology, Department of Neurology at Johns Hopkins Hospital in Baltimore, Maryland.
